INVITE US INTO YOUR INBOX
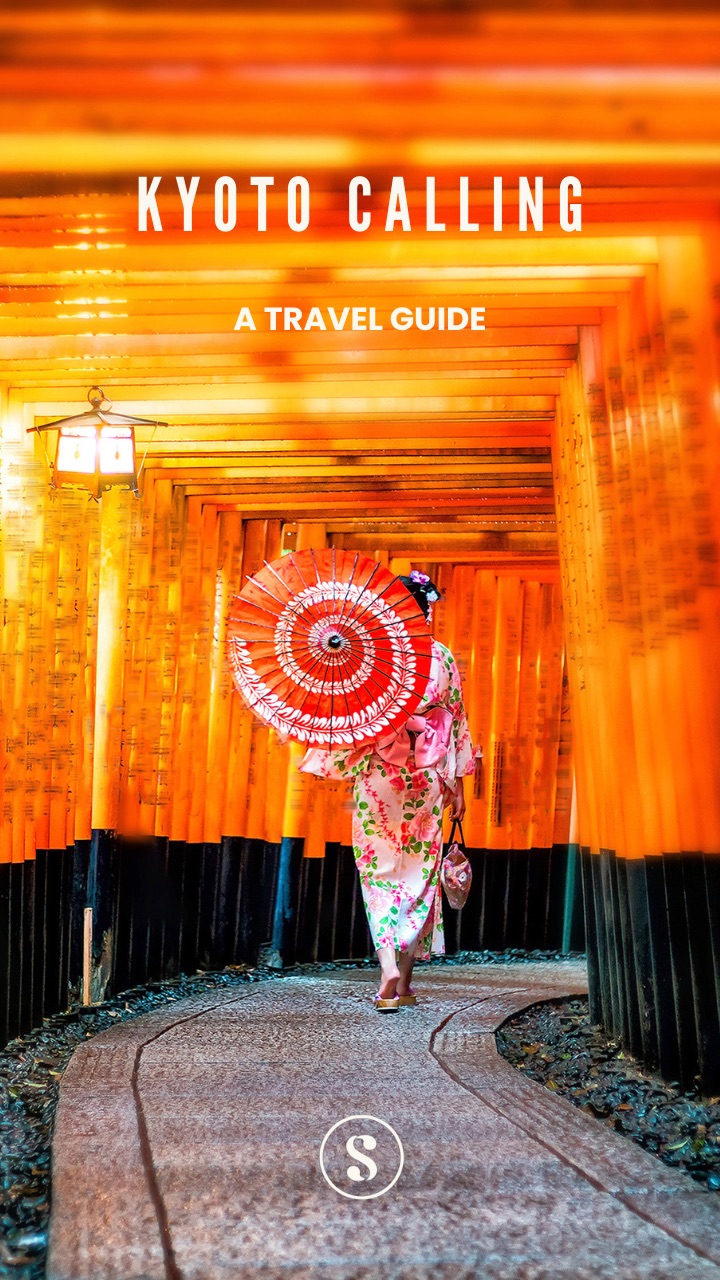
Sign up for Advisory! It’s free and so is our exclusive
welcome
aboard travel guide to Kyoto.
Our weekly goodie bag includes:
- Carefully curated lists on what to watch, read or listen to.
- Unique essays on art, history and pop culture.
- Best reads across the world (w/ gift links)
- Reading guide to the biggest news stories.
- Authentic, cool, tasteful shopping recommendations.
What you won’t get: Spam or AI slop!
Already a user ? Login
Privacy Policy. You can unsubscribe any time.Almost done!
Tell us a bit more about yourself to complete your profile.
You're subscribed!
Thank you for joining our community.